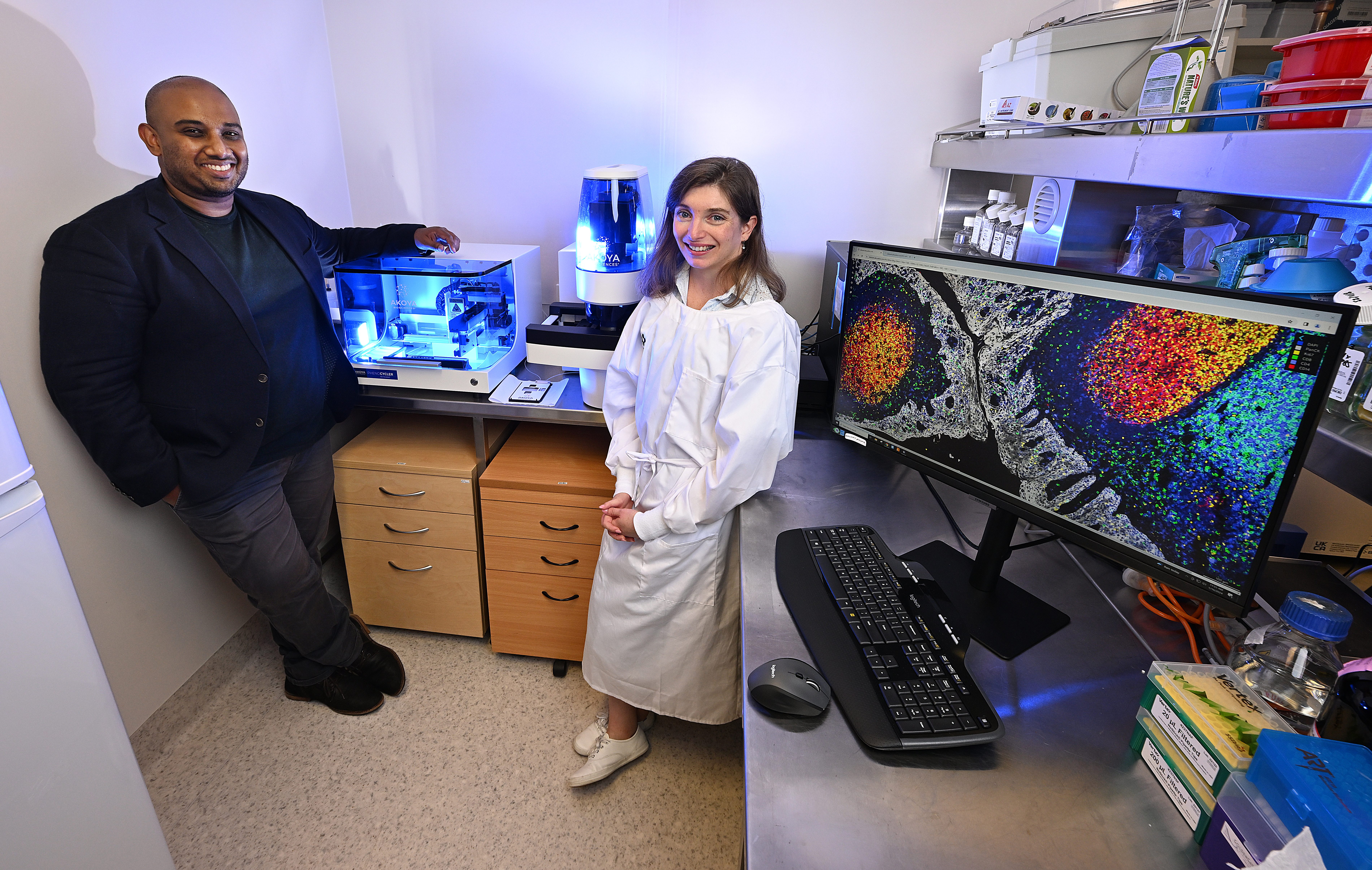
In an incredibly exciting development Arutha Kulasinghe will take his promising spatial biology research from tumour samples to blood samples, all thanks to Foundation funding.
The blood proteomic (study of proteins) project will be based on lung cancer patients and will take the same ‘google maps’ approach Associate Professor (A/Prof) Kulasinghe and his team have taken in solid tumour samples and apply it to blood samples.
Funding from the Foundation’s donors has enabled Arutha to employ a research officer to collect and build a biobank of samples from which to obtain crucial cancer biomarkers.
Once the samples are taken, A/Prof Kulasinghe’s lab can apply next generation technologies to study the blood samples and identify what story the proteins in the blood are telling them about the patient’s cancer.
Two important aspects of the work are the fact that taking blood samples as opposed to taking tumour samples is much less invasive for the patient themselves, as well as the fact blood samples can be taken at each check-up. Tracking blood based biomarkers in the blood allows us to see how the cancer is evolving during therapies, providing a real-time snapshot of the tumour dynamics.
“Having a dedicated research officer to build our biobank allows us to meticulously collect, process and biobank clinical samples over the course of therapy at the PA Hospital. That then enables us to profile thousands of circulating proteins using these cutting-edge technologies,” A/Prof Kulasinghe said.
“The goal is to measure many hundreds to thousands of proteins to identify biomarkers that may be predictive of clinical outcome, because then you know that when a lung cancer patient comes in, from studying the diagnostic blood sample we can predict if the patient is likely to develop cancer recurrences or spread to other organs. These ultimately provide medical oncologists new tools to understand and track disease using a simple blood draw.
Though the study is in lung cancer, a field where Arutha’s work in solid tumours has made significant breakthroughs, Arutha said the research can apply to others forms of cancer as well. Vitally, he believes it will be key to picking up cancer at earlier stages, leading to improved outcomes and saved lives.
“We’re going to develop these assays in lung, but we can parallel the work in breast, in prostate, melanoma, and aggressive forms of skin cancer, etc.,” he said.
“The global oncology community is struggling to detect early-stage cancers, right? So, we need more biomarkers to identify stage one and stage two patients, where the volume of disease is low and what’s shedding into the blood is at a low concentration. If we can identify protein biomarkers associated with earlier stage disease, this allows us detect and potentially treat patients sooner, ultimately leading to better patient outcomes.
“When you detect tumors at stage four, you've got limited options. When you detect it at earlier stages of disease, you tend to have better outcomes, and more therapeutic options. Our question here is, can we identify biomarkers in the blood that stratify with therapeutic outcomes, but also are these biomarkers useful for early-stage cancer detection? It is an ongoing challenge for the field.
“The challenge for the field of liquid biopsy has been that there's been limited amounts of information that you can get from the blood, right? Generally, you look for mutations, but then you don't really know what mutations to look for, which are tumour specific. What we wanted to do, working with Professor Ken O’Byrne and a few other oncologists at the PA, was to do a protein screen of the bloods for biomarkers associated with different therapeutic outcomes.
“This has evolved because the technologies have now developed to be able to look at not just, 10 or 20 or 50 proteins, but almost 10,000 different proteins in the blood. So, it's trying to put a discovery biology lens on clinical samples to see what are the proteins that can be found in the blood that might be predictive of therapeutic outcome.”
“These new technologies allow us to look at thousands of proteins within 10 microliters, which is the smallest, tiniest amount of blood, and from that we can look at thousands of protein biomarkers.
“What this project enables us to now do is to collect samples from the PA from lung cancer patients at diagnosis. Patient blood is taken again at six weeks after therapy, 12 weeks, 18 weeks, 24 weeks, and it keeps going. All we do is take a single blood tube at each time point, and now we can look at 10,000 different biomarkers over the course of therapy.
“That's really useful because we can see, what are the proteins that are changing with patients that are progressing, or what are the proteins that are decreasing in patients that are doing well, and are there a biomarker in there that will predict for patients that are cured of lung cancer or those patients that are likely to develop recurrences.”




